Introduction
Artificial Intelligence (AI) is making significant strides in healthcare, particularly in predicting outcomes for brain surgery in patients with high-grade gliomas. A recent study led by Patrick Luckett, PhD, at Washington University School of Medicine in St. Louis, MO, has demonstrated how combining machine-learning algorithms with resting-state functional MRI (fMRI) can provide highly accurate predictions of surgical outcomes. This blog explores the study’s findings and the potential implications for improving patient care and surgical planning.
The Synergy of AI and Resting-State fMRI
Background and Approach
High-grade gliomas are among the most common and aggressive brain cancers, accounting for 60% to 70% of new cases with a median survival time of 14 months. Treatment typically involves surgical tumor removal, which can lead to significant functional and cognitive deficits, followed by radiation and chemotherapy. Traditional brain mapping methods using “task” fMRI require patient participation in specific tasks, which is not always possible.
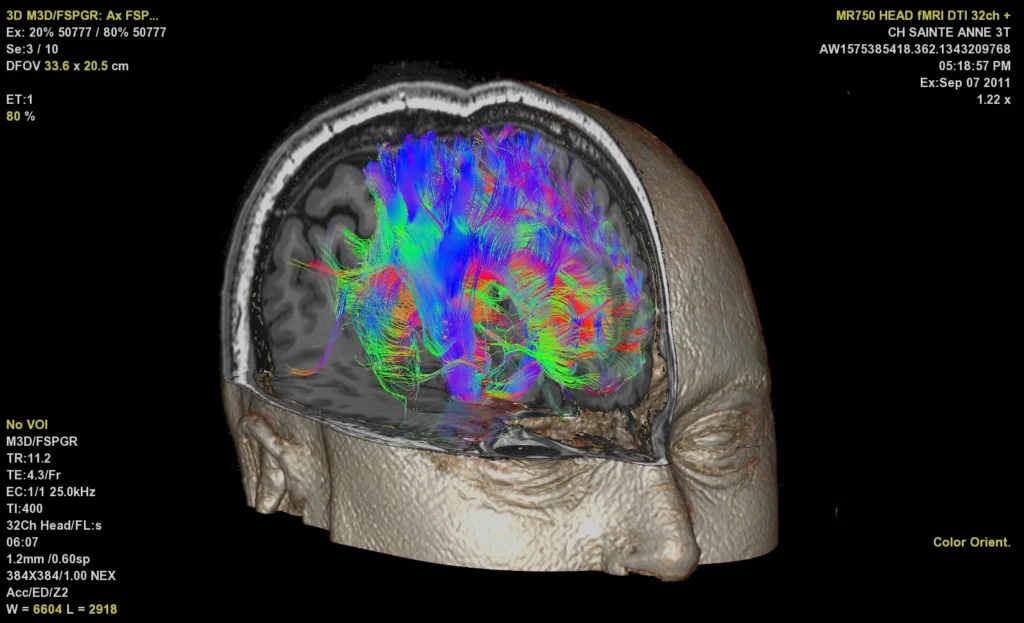
Resting-state fMRI provides an alternative by examining the brain’s intrinsic functional connectivity without requiring task performance, making it feasible to conduct even under sedation. This method allows for the simultaneous mapping of multiple brain networks, offering a comprehensive view of brain function.
Study Insights
Using resting-state fMRI data, the research team created a random-forest classifier to predict brain surgery outcomes in glioma patients. Published on May 24 in the Journal of Neuro-Oncology, the study involved 102 patients from the neurosurgery brain tumor service at Washington University Medical Center. These patients underwent structural neuroimaging and resting-state fMRI before surgery. The team utilized demographic information, connectivity measures, tumor location, and tumor volume to train their AI model, which predicted functional outcomes measured by the Karnofsky Performance Status (KPS) scale, assessing a patient’s ability to perform daily activities.
Key Findings and Results
Model Accuracy
The AI model achieved an accuracy of 94.1% and an area under the receiver operating curve (AUC) of 0.97 in predicting post-surgical functional outcomes, demonstrating its potential to significantly enhance predictive capabilities in clinical settings.
Significant Predictors
The study identified several key factors that strongly predicted surgical outcomes:
- Connectivity Quality: The quality of resting-state network connectivity between somatomotor, visual, auditory, and reward networks.
- Tumor Positioning: The relationship of the tumor to networks such as dorsal attention, cingulo-opercular, and basal ganglia.
- Patient Characteristics: Age at diagnosis and overall survival duration were linked to poorer outcomes.
- Medical History: Higher incidences of hypertension, hyperlipidemia, and seizures were associated with worse outcomes.
- Tumor Volume: Found to be a moderate predictor of functional outcomes.
Practical Implications for Patient Care
The integration of AI with resting-state fMRI to predict surgical outcomes offers numerous benefits:
- Optimized Surgical Planning: Provides surgeons with detailed predictive information to balance long-term survival prospects with potential recovery challenges.
- Improved Patient Communication: Helps set clearer expectations for patients regarding their treatment outcomes.
- Customized Rehabilitation Programs: Informs the need for personalized rehabilitation services such as physical, occupational, or speech therapy based on predicted KPS scores.
- Tailored Monitoring and Follow-Up: Facilitates individualized follow-up plans, including visit frequency and quality of life assessments.
- Targeted Support Services: Guides the provision of mental health interventions and family counseling to manage the emotional aspects of high-grade glioma care.
Conclusion
The study spearheaded by Dr. Patrick Luckett and his colleagues showcases the transformative potential of AI and resting-state fMRI in predicting brain surgery outcomes. This innovative approach not only enhances surgical planning and patient care but also paves the way for more personalized treatment strategies for high-grade gliomas. As AI technology continues to evolve, its application in medical imaging promises to further improve patient outcomes and overall quality of life.